
Can Physiotherapy Help Arthritis? Let’s find out
While there’s no one-size-fits-all cure for arthritis, physiotherapy has emerged as a powerful, non-invasive approach to managing symptoms, improving function, and empowering individuals to regain control over their lives.
Understanding the Impact of Arthritis
Arthritis isn’t a single disease; it’s an umbrella term encompassing over 100 different conditions that affect the joints. The two most prevalent types are:
- Osteoarthritis (OA): Often referred to as “wear and tear” arthritis, OA is the most common form. It develops gradually as the cartilage, the protective cushion between bones, breaks down, leading to pain, stiffness, and reduced joint mobility.
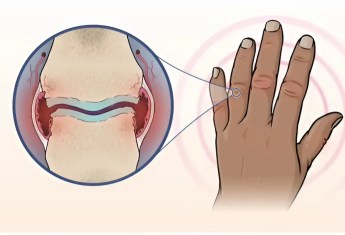
- Rheumatoid Arthritis (RA): RA is an autoimmune disease in which the body’s immune system mistakenly attacks the lining of the joints (synovium), causing inflammation, pain, stiffness, and eventually joint damage. Unlike OA, RA can affect multiple joints simultaneously and often presents with systemic symptoms like fatigue and fever.
The symptoms of arthritis can vary widely depending on the type and severity, but common complaints include:
- Pain in the affected joints
- Stiffness, especially in the morning or after periods of inactivity
- Swelling around the joints
- Limited range of motion
- Muscle weakness
- Fatigue
These symptoms can significantly impact an individual’s ability to perform daily activities, work, engage in hobbies, and maintain their independence. Simple tasks like walking, climbing stairs, dressing, or even gripping objects can become challenging and painful.
How Physiotherapy Empowers You to Move Better
Physiotherapy focuses on restoring and maintaining movement and function, playing a pivotal role in arthritis management. It aims to:
- Reduce pain and inflammation: Through a combination of therapeutic exercises, manual therapy, and modalities like heat or cold therapy.
- Improve range of motion and flexibility: By gently stretching tight muscles and mobilizing stiff joints.
- Strengthen muscles around affected joints: Stronger muscles provide better support and stability for joints, reducing pain and improving function.
- Improve balance and stability: This is especially important for individuals with arthritis, as joint pain and stiffness can increase the risk of falls.
- Enhance functional mobility and independence: Physiotherapy helps individuals regain the ability to perform daily activities with greater ease and confidence.
Physiotherapists take a personalized approach, tailoring treatment plans to each individual’s specific needs, limitations, and goals. A comprehensive assessment is the foundation of this process, involving:
- A detailed discussion of the individual’s medical history, symptoms, and functional limitations.
- Physical examination to assess joint range of motion, muscle strength, flexibility, balance, and posture.
- Discussion of the individual’s goals and expectations for physiotherapy.
Based on this assessment, the physiotherapist collaborates with the individual to develop a personalized treatment plan that outlines specific exercises, manual therapy techniques, and other modalities to address their unique needs.
Physiotherapy Tools and Techniques
Physiotherapists employ a variety of evidence-based techniques to manage arthritis and improve function, including:
Therapeutic Exercises
Exercise is considered a cornerstone of arthritis management, helping to maintain joint mobility, strengthen supporting muscles, reduce pain, and improve overall fitness. Physiotherapists prescribe specific exercises tailored to the individual’s needs and abilities. These may include:
- Range-of-Motion Exercises: These exercises involve moving the affected joint through its full range of motion to prevent stiffness and maintain flexibility. For example, heel slides are commonly prescribed for knee osteoarthritis to improve knee flexion and extension.
- Strengthening Exercises: Strengthening the muscles around the affected joints is crucial for providing support and stability. Examples include squats, glute bridges, and straight leg raises.
- Low-Impact Aerobic Exercise: Aerobic exercise improves cardiovascular health and overall fitness without putting excessive stress on the joints. Suitable options include swimming, cycling, or water exercises.
- Balance Exercises: Exercises that challenge balance help improve stability and reduce the risk of falls. Physiotherapists may incorporate exercises like standing on one leg, walking heel-to-toe, or using a balance board.
Manual Therapy
Manual therapy involves skilled hands-on techniques performed by the physiotherapist to mobilize joints, release muscle tension, and reduce pain. Commonly used techniques include:
- Joint Mobilization: Gentle, rhythmic movements applied to the joint to restore normal mechanics, improve mobility, and reduce stiffness.
- Soft Tissue Mobilization: Techniques like massage, stretching, and trigger point release to address muscle tightness, improve circulation, and reduce pain.
Other Modalities
Physiotherapists may also incorporate other modalities to complement exercise and manual therapy, including:
- Heat and Cold Therapy: Applying heat can help relax muscles and reduce stiffness, while cold therapy can help reduce pain and inflammation.
- Transcutaneous Electrical Nerve Stimulation (TENS): TENS uses low-voltage electrical currents to stimulate nerves and reduce pain signals.
- Acupuncture: Acupuncture involves inserting thin needles into specific points on the body to stimulate healing and relieve pain.
Assistive Devices
When necessary, physiotherapists can recommend and train individuals to use assistive devices to improve mobility, safety, and independence. These may include canes, walkers, crutches, braces, or orthotics.
Long-Term Management and Self-Care Strategies
Physiotherapy empowers individuals to take an active role in their arthritis management. Beyond in-clinic treatments, physiotherapists emphasize long-term self-care strategies, including:
The Importance of Rest and Recovery
While exercise is essential, adequate rest and recovery are equally important, especially for individuals with inflammatory types of arthritis like RA. Overexertion can exacerbate inflammation and lead to setbacks. Physiotherapists guide individuals in finding the right balance between activity and rest, emphasizing the importance of listening to their bodies and modifying activities as needed.
Developing a Home Exercise Program
Physiotherapists work with individuals to create personalized home exercise programs to maintain progress and prevent setbacks. These programs typically include a combination of range-of-motion, strengthening, and low-impact aerobic exercises, tailored to the individual’s abilities and goals. Adhering to the home exercise program is essential for long-term success.
Lifestyle Modifications
Simple lifestyle changes can go a long way in managing arthritis. Physiotherapists offer practical advice on:
- Maintaining a Healthy Weight: Excess weight puts extra stress on joints, particularly weight-bearing joints like the knees and hips. Losing even a small amount of weight can significantly reduce pain and improve function.
- Ergonomics and Joint Protection: Using proper techniques for lifting, carrying, and performing daily tasks can minimize stress on joints. Physiotherapists provide guidance on ergonomics at work, at home, and during recreational activities.
- Pacing Activities: Learning to pace activities and avoid overdoing it is crucial for preventing flare-ups and managing fatigue. Physiotherapists help individuals develop strategies for breaking down tasks, alternating between activities, and incorporating rest breaks throughout the day.
Managing Flare-ups
Flare-ups are periods when arthritis symptoms worsen. Physiotherapists educate individuals on how to recognize early warning signs and take steps to manage flare-ups, including:
- Rest: Reducing activity and resting the affected joint is often the first step.
- Ice or Heat Therapy: Applying ice can help reduce inflammation and pain, while heat can help relax muscles and reduce stiffness.
- Medication: Over-the-counter pain relievers or prescription medications may be necessary to manage pain and inflammation.
- Modifying Activities: Adjusting activities to avoid movements that aggravate the joint can help reduce pain.
- Consulting with a Physiotherapist: If a flare-up is severe or doesn’t improve with home management, it’s important to consult with a physiotherapist for further guidance.
Benefits of Early Intervention
Early intervention with physiotherapy is crucial for achieving the best possible outcomes for arthritis.
- Early Diagnosis: If you experience persistent joint pain or stiffness, don’t delay seeking medical attention. Early diagnosis allows for prompt treatment and can help prevent further joint damage.
- Preventing Further Damage: Physiotherapy can help slow the progression of arthritis and prevent or minimize joint damage, preserving function and mobility.
- Improving Outcomes: Starting physiotherapy early can lead to better overall outcomes, including reduced pain, improved function, and a higher quality of life.
Take the First Step Towards a More Active Life
If you’re living with arthritis, physiotherapy can be your partner in managing pain, improving function, and enhancing your overall well-being. Don’t let arthritis hold you back from the activities you enjoy. Consult with a qualified physiotherapist today to start your journey towards a more active and fulfilling life.
